"In a real sense, a wheelchair is an extension of the user's body. Therefore, it is critical that any prescription for a new wheelchair must match the user's current expectations, preferences, physical needs and functional requirements that emerge out of his or her interactions with the environment1."

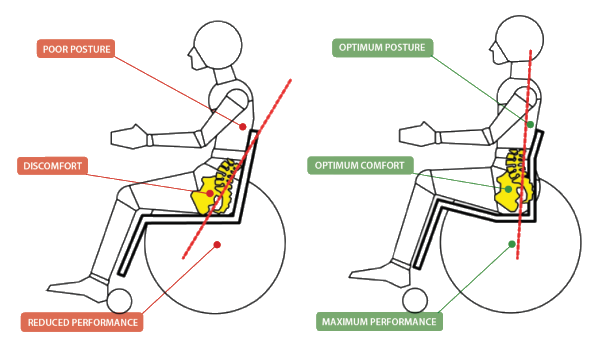
Sitting all day is hard work! It is even harder if you sit in a wheelchair all day. Long-term sitting has been shown to result in poor posture, the impact of which is often associated with:
- Muscle fatigue
- Contractures and spasticity
- Poor systemic function
- Immobility
- Increased pain and discomfort
- Tissue trauma
- Increased dependency
To ensure best fit of mobility and seating systems, and to promote optimal participation and function, there is a process that can be followed to optimise outcomes. This process is followed by your prescribing therapist and is recommended prior to all wheelchair prescriptions.
This process is call the MAT Assessment - Mechanical Assessment Tool (MAT) or MAT Evaluation - which gathers a comprehensive client profile. It enables the therapist to determine optimal position of the client, which will promote postural efficiency, and enhanced seating ability. The MAT Assessment enables seating interventions to be individualised to meet the distinct and unique needs of each individual client, including functional capacity, posture, and pressure management.
Studies2 indicate that clinically prescribed seating systems help promote:
- Good posture
- Greater muscle efficiency
- Participation in activities – encouraging learning, socialising, independence
- Promote function and participation
- Enhanced organ activity
The value of using the Mechanical Assessment Tool (MAT)
A MAT assessment is used by seating clinicians as part of the seating assessment process. The MAT Assessment may also be referred to as a biomechanical assessment or a physical evaluation where information about a person's seating capacity is gathered – for example:
- Muscle tone and muscle spasm patterns
- Range of motion
- Joint flexibility
- Muscle length
- Skeletal alignment
The information collated in this session will reflect requirements for mobility bases choice, sizing of backrests, seat cushions, wheelchair widths; and postural supports that may be required. Results of the MAT Assessment should assist in finding the optimal seating position to promote function, participation and comfort.
Conducting the MAT Assessment
There are 5 key stages to a MAT Assessment:
- Information gathering – client’s history, diagnosis, surgical history, previous mobility and seating experiences, goals etc.
- Supine lying assessment – assess and record information about alignment, muscle length and symmetry, flexibility of joints, and where to correct or accommodate posture discrepancies.
- Sitting assessment – assess sitting ability, balance, stability, symmetry, head control, and position of the limbs of the client in the seated position.
- Simulate new posture and Centre of Gravity - simulate the optimal posture, and determine the best centre of gravity for the user.
- Measurements taken – full body measurements are taken of the client whilst seated in the optimal position – these are recorded to ensure optimal set up of the chair’s seating system.
The client is observed in a supine lying position, and then again, sitting on a firm surface, such as a plinth. Observing the client in these positions helps gather information about the client’s posture and alignment and how these may affect the seating posture when seated. The pelvis is the foundation for sitting as it supports the person’s body weight. Pelvic positioning will affect the alignment of the trunk, head, upper and lower extremities. Generally, when a client is fitted into a new wheelchair seating system, the process is evaluated according to sequential steps noted above to ensure a successful result.
Optimal Sitting Posture
The goal of seating is to find 'that posture and position' in which the spine is least affected by gravity, and the least effort is required to maintain an upright straight, and symmetrical seating position. The optimum seating position will vary for each person, and must be guided by the findings from the MAT Assessment.
The following is a guideline to the sequence of seating for optimal positioning, comfort and sitting tolerance:
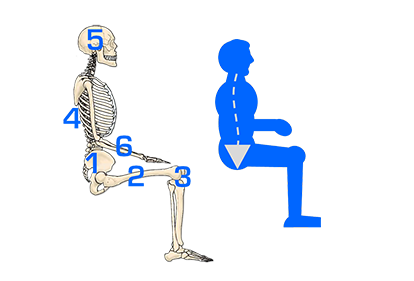
1. PELVIS
The pelvis is the largest and heaviest boned in the body. It should be positioned and stabilised first for optimal symmetrical alignment.
2. HIPS & THIGHS
Wind-sweeping, internal or external femoral rotation is often affected by the position of the pelvis. Failing to accommodate wind-sweeping can increase rotation and asymmetrical shaping in the torso region. Correct sitting position can also help alleviate hip dislocation, subluxation and tightened hamstrings.
3. KNEES & FEET
Positioning of the knees and feet correctly (preferably at 90º) also helps to stabilise the pelvis in the seat.
4. ARMS
The position of the arms help support the torso and can affect a person's centre of gravity. Upper arms should be relaxed and in line with the torso. If the forearms are too far back on the armrest, shoulders may become retracted. Armrests positioned too high can cause painful shoulder elevation. Armrests which are too low reduces head control and may increase the risk of a kyphosis, reducing spinal extension.
GRAVITY
It is also important to remember the impact of gravity on all seating assessments. Gravity is a powerful force on an unsupported body, which over time can have a devastating effect on posture.

Resources: The Agency for Clinical Innovation (Spinal Seating Modules) is a good resource if you would like to find out more about MAT Evaluations. (Agency for Clinical Innovation - (https://www.aci.health.nsw.gov.au/networks/...3/the-mechanical-assessment-tool-mat).
Clinical Diagrams: The Science of Seating. Dreamline Seating Solutions https://www.rolapal.co.nz: RGK Wheelchairs.
Images: Sunrise Medical; Rolapal NZ
References:
1(Batavia M, Batavia AI & Friedman R. 2001. Changing chairs: anticipating problems in prescribing wheelchairs. Disabil Rehabil. Aug 15; 23(12): 539-48).
2(Sprigle S, De l’aune W. 2013. Factors contributing to extended activity times during the provision of wheeled mobility devices. Disabil Rehabil Assist Technol. 2013 May:8(3):225-31. doi: 10.3109/17483107.2012.71343).


















